Did you know there are an estimated 3,000 mobile clinics in the United States serving about 10 million visits every year? That sounds like a lot at first, but when you think about how big this country is and how many people struggle to reach care, it suddenly feels small.
If you work in healthcare, you’ve probably felt this shortage firsthand. Maybe your team can’t reach enough patients in rural counties. Maybe city programs are stretched thin, leaving people waiting weeks for basic screenings. That gap leaves you frustrated and worried about the long-term health of the people you serve.
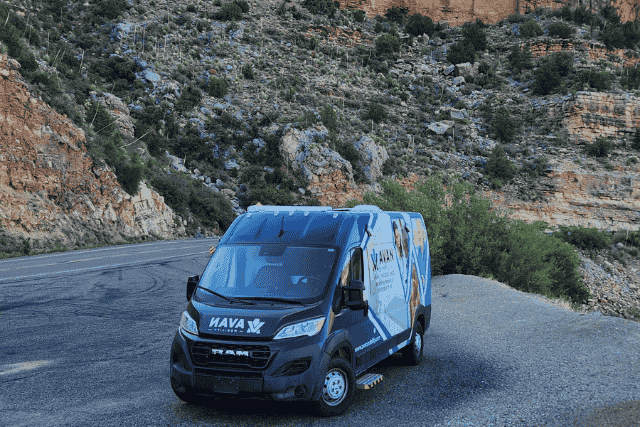
At AVAN Mobility, we understand the weight you carry. For more than 10 years, we’ve built over 150 mobile medical units, working with groups like the Community Clinic of Southwest Missouri and Pacific Clinics. We’re Ford QVM and Stellantis QPro certified, and our vehicles are trusted by healthcare networks, non-profits, and local governments across the country.
We take pride in listening to what makes your community unique before building anything, because no two programs are ever the same. And while we know we’re not the only manufacturer, we’re proud to be part of the solution.
In this article, you’ll learn:
- If there really is a shortage of mobile medical clinics in the U.S.
- How this shortage impacts healthcare programs and patients across the country
- What steps you can take to start closing the gap
What’s the data say about the shortage of mobile clinics in the U.S.?
Yes, there is a shortage of mobile clinics in the U.S.
The U.S. has about 335 million people. Spread across a country this size, you’d think mobile healthcare would be everywhere, but it’s not. As we mentioned earlier, approximately 3,000 mobile clinics operate nationwide. These clinics provide around 10 million visits a year. That sounds like a lot, until you compare it to the need.
Why are 3,000 mobile clinics not enough?
- Population vs. Clinics: 335 million people divided by 3,000 clinics equals about 111,000 people per mobile clinic. That’s like one clinic being responsible for an entire mid-sized city.
- Rural Gaps: Nearly 46 million Americans live in rural areas. Many of these areas don’t even have a hospital. Mobile clinics could fill that gap, but with only 3,000 spread across the whole country, the coverage falls short.
- Urban Demand: It’s not just rural America. In cities, people without housing, people living in poverty, and underserved neighborhoods all rely on mobile healthcare. With rising demand, 3,000 clinics can’t keep up.
State-level snapshots
Some states highlight the shortage even more clearly:
| State | Number of mobile clinics in Mobile Health Map | What this means for local/far-flung populations |
| Nevada | 1 clinic | Very sparse → remote communities likely wait long to get services. |
| Wyoming | 2 clinics | Huge land area to cover, low population density → big travel distances. |
| Montana | 4 clinics | Many towns are isolated, and clinics are often far apart. |
| Alaska | 2 clinics | Harsh conditions add barriers. |
| Texas | 61 clinics | Better numbers, but rural sectors are still underserved. |
| California | 120 clinics | Has many, but population and geography mean gaps remain. |
Mobile clinics are useful tools for reaching people who would otherwise go without care. But as you can see from these numbers, 3,000 units for 335 million people is not enough. Demand is growing faster than supply, and the gap is most painful in rural states and underserved city communities.
How does the shortage of mobile clinics impact healthcare programs?
When there are too few mobile medical units, both healthcare programs and real people suffer. Programs struggle to serve, and patients end up paying the price, sometimes literally with their health.
- Reduced reach: According to the Mobile Health Map study, about one-third of mobile clinics serve rural or frontier communities. That means many programs cannot reach remote areas often enough.
- High cost per outcome: When clinics are far apart, travel, fuel, staffing, and logistics costs go up fast. If a clinic only visits a remote town once a month, things like preventive screenings or chronic disease check-ups don’t happen regularly. Delayed diagnosis means worse cases later, which cost much more to treat.
- Overload on fixed facilities: Without mobile clinic support, local hospitals or clinics get hit with patients whose conditions have worsened. Emergency rooms fill with issues that could’ve been handled earlier. That stresses staff, drives up costs, and reduces the quality of care. Research finds that many rural areas have increased mortality and poorer health outcomes linked to these access gaps.
- Missed funding or support opportunities: Programs built on grant dollars or Medicaid/Medicare reimbursements need proof of impact. When mobile clinic numbers are thin, data are sparse. If your program can’t show consistent service in rural or underserved zones, you may lose funding or political support.
How does a shortage of mobile clinics affect patients?
Imagine Marie, 70, has kidney disease and needs dialysis three times a week. She’s lived in a small town in Arizona for 30 years. The nearest hospital that can do dialysis is five hours away by car. That’s ten hours round trip, three times a week. Over a month, that’s about 120 travel hours. Her gas, lodging, time off work (or time caring for family), and physical toll are enormous.
Because of that, Marie sometimes misses sessions. Missing dialysis means toxins build up in her body. She ends up in the ER more, her quality of life drops, and she risks serious complications like infections or heart problems. If there were more mobile clinics equipped to provide some dialysis support or closer chronic kidney disease management, Marie might stay healthier, avoid ER visits, and sleep better.
Other everyday examples:
- A parent in rural Alabama whose child has asthma: no clinic nearby means poor control, more hospital visits, maybe more missed school.
- A pregnant woman in Montana who must travel long distances for prenatal care: missed appointments, risks for mom and baby rise.
What does all of this mean?
If your organization is trying to serve high-need communities:
- You may be trying to stretch one mobile clinic to far-flung towns. That means fewer visits, longer travel, higher burnout among staff.
- Patients may show up sicker, later. Preventive care and chronic disease management suffer. That makes your outcomes worse, even if you try.
- Funding bodies will ask for proof of impact. If the data are inconsistent because your service is too sparse, you may lose grants or support.
How can your healthcare organization start closing the shortage gap of mobile clinics in the U.S.?
If you’re a healthcare organization that has seen these numbers and felt the pain firsthand, there isn’t a better time than now to start addressing this gap. Mobile clinics are lifelines that bring care to people who would otherwise go without. And every step you take can make a real difference for patients and communities.
Here are five actionable steps you can take to start closing the shortage of mobile clinics:
1. Research your communities and neighboring areas
Start by mapping where your patients live and how far they have to travel for care. Look at rural counties, medically underserved urban neighborhoods, and communities with high rates of chronic illness or uninsured residents.
How to do it:
- Check HRSA Health Professional Shortage Area data for your state and neighboring counties.
- Talk to local public health departments, hospitals, and clinics about gaps they see in care.
- Identify the patient populations most at risk, like seniors with chronic conditions, children with asthma, or pregnant people in rural zones.
2. Identify your most critical services
Once you know the areas of highest need, decide which services will have the biggest impact.
Mobile clinics can offer a wide range of options:
- Preventive screenings
- Chronic disease management
- Mental health counseling
- Maternal care
- Vaccinations
Tip: Focus first on services that prevent serious complications or repeated ER visits.
For example:
- Regular healthcare check-ins for patients with health concerns living far from hospitals.
- Vaccination drives in underserved neighborhoods.
- Mobile prenatal care in rural counties.
3. Explore partnerships and funding opportunities
Many organizations have succeeded by partnering with local hospitals, non-profits, government programs, or even other mobile clinic operators. Funding can come from grants, Medicaid programs, or philanthropic organizations.
Examples:
- State health departments often provide funding for mobile health outreach.
- Community health foundations may help cover staffing or operational costs.
- Collaborative agreements with nearby clinics can help you share resources like medical staff or equipment.
4. Start small, scale strategically
You don’t have to launch a massive fleet overnight. Start with one mobile medical unit focused on the highest-need community. Track your impact carefully, then expand as you learn.
Imagine starting a mobile medical unit serving a rural county in Arizona. You can schedule weekly visits to remote towns, focusing on diabetes and kidney care. Over three months, you’ll collect data on patient visits, health improvements, and community response. That gives you the evidence needed to justify adding a second unit or expanding service areas.
5. Measure impact and adjust
Track patient outcomes, number of visits, missed care, and overall health improvements.
Use this data to:
- Adjust routes and schedules for efficiency.
- Advocate for additional funding or new mobile units.
- Show stakeholders and funders that your program is effective.
Tip: Even small wins matter. Helping just 50 patients a week in a rural county can prevent serious complications and reduce hospital ER visits. Over a year, that adds up to thousands of people helped.
Why is it so important to start now?
The shortage of mobile clinics isn’t going away. Aging populations, rural healthcare gaps, and underserved urban areas mean demand is only growing. Taking some of these steps now gives your organization a chance to close gaps before more patients fall through them.
Every mobile clinic and every patient reached brings us closer to a future where healthcare is truly accessible for all.
Got any questions about starting a mobile clinic in the U.S.?

You came to this article because you’ve felt the strain of the shortage of mobile clinics in the U.S. firsthand. Maybe your patients are missing care, your staff is stretched too thin, or your community simply doesn’t have enough access to timely healthcare. You wanted answers and actionable guidance, and that’s exactly what we’ve covered here.
After reading this article, you now know:
- The current gap: How the shortage of mobile medical units leaves communities underserved and patients at risk.
- The impact: Real stories and numbers showing the strain on healthcare programs and patient health.
- How to start closing the gap: Practical steps your organization can take to bring mobile clinics to the areas that need them most.
At AVAN Mobility, we’ve spent over a decade designing mobile clinics to help healthcare teams like yours save lives all over the U.S. We’re proud to help healthcare organizations expand access, reduce patient risk, and make care more reachable for everyone. If you have questions or want to explore solutions for your community, click the button below to talk to one of our mobility experts today.
If you’re not ready to speak with a mobility expert yet, here are a few resources to help you keep learning:
1. How much does a mobile medical unit cost in the U.S.? Understand the investment required to launch a mobile clinic.
2. Top 5 ways a mobile clinic vehicle improves medical accessibility: Learn how mobile medical units increase patient access and reduce gaps in care for underserved populations.
3. 10 steps to starting a mobile medical clinic: A practical guide to planning and launching your first mobile clinic, perfect for taking action after understanding the shortage.