Have you thought about what untreated opioid use disorder (OUD) really costs your community? It is more than hospital bills. Across the U.S., this crisis costs billions every year in lost work, crowded ERs, and broken families. If you run a health program, you likely see the gap every day. Patients want help but cannot find it. Waitlists are long. Overdoses happen while people sit on the sidelines. It feels heavy. But picture a different future, one where more people are able to access timely care in ways that fit their needs, and those costs start to shrink.
At AVAN Mobility, we have been building mobile medical units for more than 10 years. Health networks, counties, and non-profits across the U.S. trust us to create vehicles that bring care to people who need it. Organizations like CalOptima in California and the Community Clinic of Southwest Missouri use our solutions to reach more people. Every program is different, so we design around your needs, not ours. And while we know we are not the only manufacturer out there, our focus has always been the same as yours: Saving lives and removing barriers to care.
In this article, you will see:
- Hidden costs: What untreated opioid use disorder really costs the U.S.
- Barriers: Why people struggle to get treatment
- Action steps: How your organization can close the gap
- Impact: What changes when care arrives sooner
What do the numbers say about untreated opioid use disorder?
When opioid use disorder goes untreated, the price tag shows up everywhere. Hospitals feel it, the justice system feels it, and your community budget feels it. The numbers are staggering, and they continue to grow.
- Nationwide toll: In 2017, the total cost of OUD was $471 billion, with fatal overdoses adding another $550 billion. That’s over $1 trillion in a single year across healthcare, lost productivity, criminal justice, and quality of life.
- Per person impact: Each case of OUD costs an average of $221,000. That breaks down to:
- $14,700 in healthcare
- $7,000 in criminal justice
- $14,700 in lost productivity
- $183,000 in reduced quality of life
- Today’s reality: The numbers are even higher now. Recent research shows untreated OUD costs nearly $700,000 per case each year when factoring in the full strain on healthcare, employers, and public resources.
Every untreated case drains hundreds of thousands of dollars that could be invested in housing, education, or community development. Instead, that money gets spent reacting to emergencies, court cases, and preventable tragedies.
The human cost: These dollars represent more than budgets. They represent families torn apart, children entering foster care, and communities facing higher crime rates. When treatment doesn’t reach people in time, everyone pays.
Next, we’ll talk about the barriers that stop people from getting opioid use disorder treatment and why so many never receive help.
What barriers prevent people from getting treatment for opioid use disorder?
Even though treatment for opioid use disorder can save lives, many people never get it. Many of the biggest barriers aren’t medical at all; they’re about access, perception, and location. Let’s start with one of the hardest: Stigma.
Stigma: A silent wall between people and care
Stigma is often the biggest reason people avoid treatment for opioid use disorder. Too many still see OUD as a moral failure instead of a medical condition. That judgment shows up in whispers at the grocery store, side glances at the clinic, or even bias within the healthcare system itself. For someone already struggling, the fear of being labeled “an addict” can feel heavier than the illness.
That shame drives people to hide their condition, skip appointments, and stay silent until a crisis forces them into the ER. Rural towns and small communities across the U.S. see this even more, where “everyone knows everyone.”
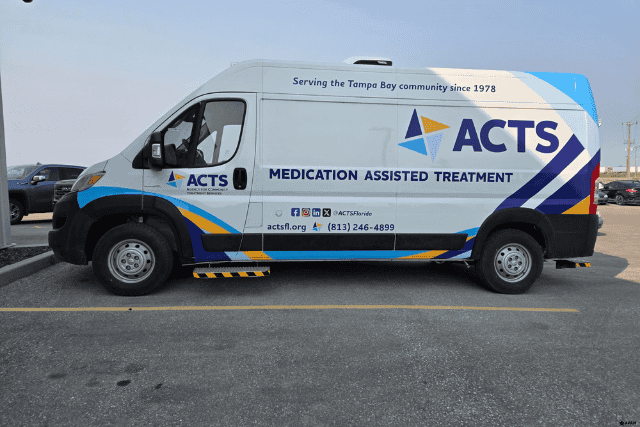
Mobile medication-assisted treatment (MAT) units help break down this wall. They can help address this challenge by providing discreet access to treatment closer to home. This may also include counseling or other supportive services.Treatment starts to feel private, approachable, and free of judgment.

Transportation: Too far, too difficult
For many people with opioid use disorder, getting to a fixed clinic is the hardest step. It’s not that they don’t want treatment, it’s that they simply can’t reach it. Rural counties across the U.S. often have only one clinic that offers medication for opioid use disorder, and it may be hours away. Without reliable transportation, that distance feels impossible.
Here’s what transportation barriers look like:
- No car: Many patients can’t afford a vehicle or gas.
- Limited transit: Buses may not run to treatment centers, or routes take too long.
- Work conflicts: A two-hour round trip means missed shifts and lost pay if the person is employed.
- Unreliable rides: Depending on friends or family adds stress and uncertainty.
Mobile health units, including those that can provide MAT, help close this gap by bringing services directly to the people. Instead of asking people to travel long distances, treatment comes to their community. Whether parked outside a community center, church, or local health office, mobile units remove the burden of transportation and turn access into something realistic.
Clinic shortages and long wait times
Even when someone is ready to start treatment for opioid use disorder, the system doesn’t always have room for them. Across the U.S., many counties don’t have enough clinics, and the ones that do exist often face overwhelming demand. Waiting weeks, or even months, for an appointment can mean losing someone to relapse or overdose before they ever get care.
Here’s how the shortage shows up:
- Limited providers: Few doctors are licensed to prescribe medication for opioid use disorder.
- Overloaded clinics: Centers can’t keep up with the volume of patients.
- Long delays: People wait weeks to begin treatment, when help is needed right away.
- Geographic gaps: Some rural counties don’t have a single treatment provider.
Mobile medical units can ease this pressure by expanding the reach of existing programs. Depending on the setup, they may provide MAT, counseling, peer support, or other services. They expand the reach of existing programs, add capacity in high-demand areas, and cut down waitlists. Mobile units bring care directly into underserved communities, transforming “come back in six weeks” into “we can start today.”

Cost and insurance challenges
Money is still one of the biggest walls between people and treatment for opioid use disorder. Even if clinics are available, the price of ongoing care can scare people away. Some patients don’t have insurance. Others have coverage but face high deductibles or limited benefits for substance use treatment. For many, the choice becomes paying rent or paying for recovery.
Here’s what those cost barriers look like:
- No insurance: Millions of Americans still fall through coverage gaps.
- High out-of-pocket costs: Copays and deductibles make treatment feel out of reach.
- Limited benefits: Some plans don’t fully cover medication for opioid use disorder.
- Hidden expenses: Transportation, time off work, and childcare add up fast.
The good news is there’s opioid settlement funding available across the U.S., but many organizations don’t realize they can use it for mobile treatment programs. A mobile MAT unit helps your team stretch those dollars further, reaching more people for less. Instead of waiting for patients to come to an expensive clinic, you can deliver care directly to them, reducing costs while expanding access.
How can treating opioid use disorder help lower these hidden costs?
Research shows that when people with OUD engage in treatment, outcomes improve. For example, medications like methadone and buprenorphine are associated with significantly lower mortality rates. Other supportive services, such as counseling, case management, and harm reduction, also play important roles in improving outcomes. A large review found over a 50 percent lower all-cause mortality while on treatment, compared to no treatment.
- Right after an overdose, speed matters: Starting buprenorphine after a nonfatal overdose was linked to a 62 percent lower risk of opioid-involved death in the following year.
- More people start and stay in care: Once treatment begins, staying engaged is easier with options like monthly extended-release buprenorphine, which showed strong retention out to 96 weeks in a recent study.
- Costs fall for your community: Economic studies show big savings when people receive medication for opioid use disorder: About $100,000 per person for methadone, $60,000 for buprenorphine, and $40,000 for extended-release naltrexone, versus no treatment.
- Crime and justice costs drop too: People who stay on opioid agonist treatment have fewer arrests than those who are untreated.
Why does mobile medication-assisted treatment for opioid use disorder change the curve?
Many people dealing with OUD never reach a fixed clinic due to some of the barriers we discussed earlier. Mobile programs that include MAT and other services bring care closer to people, helping reduce barriers and improve access.
- More starts, fewer barriers: Mobile programs have been shown to increase methadone access and may boost retention, especially for underserved groups.
- Stronger engagement: A mobile engagement unit in Philadelphia increased use of methadone maintenance and outpatient care after intake compared to usual pathways.
- Faster reach in rural counties: Mobile teams can set weekly routes to town halls, shelters, and tribal centers, so people start medication for opioid use disorder without a long trip.
What can you expect when you go mobile?
- Lower deaths: Start people on MAT for opioid use disorder sooner, and the risk of death drops. Pair mobile starts with take-home naloxone, and you protect more lives.
- Lower spend: Each person who receives opioid use disorder treatment avoids large lifetime costs tied to emergency care, crime, and lost work.
- Higher retention: Monthly injectables and flexible visit sites make it easier to stay in care.
- Safer communities: Ongoing treatment is linked to fewer arrests and more stability.
A quick reality check
Even with clear benefits, only one in four adults who needed treatment in 2022 received medications like methadone or buprenorphine. Bringing medication-assisted treatment for opioid use disorder to neighborhoods helps close that gap.
How do you fund this shift?
Many states let opioid settlement money pay for mobile treatment services, like mobile medication vans. For example, Ohio includes mobile treatment as an approved expense in its plan for using settlement funds. A recent HHS ASPE brief shows states are using settlement dollars to pay for and operate mobile medication units.
Bottom line: When treatment comes to people through mobile health services:
- More people get care
- Access improves
- Communities spend less time dealing with crises
That’s how you turn the hidden costs of untreated opioid addiction into real progress.
Got any questions about starting a mobile medication-assisted treatment unit?
You came to this article because you’ve seen the hidden toll of untreated opioid use disorder in your community. The rising costs, the lost lives, and the barriers holding people back from care all hit close to home.
Here’s what you learned today:
- The cost: Untreated opioid use disorder drains billions from the U.S. every year.
- The barriers: Stigma, transportation, wait times, and cost keep people from fixed clinics.
- The solution: Mobile medication-assisted treatment units remove those barriers and save lives.
At AVAN Mobility, we know vehicles alone don’t save lives; people do. That’s why we work alongside your team to design mobile units that fit the way you serve, not the other way around. We’ve partnered with community health programs, tribal organizations, and nonprofits across the country to turn obstacles into opportunities for care.
What makes us different is our belief that mobility is a way to bring dignity, safety, and hope to people who might otherwise be left behind. If you’re ready to explore solutions, click the button below to talk to a mobility expert today.
If you’re not ready to connect with us yet, here are a few resources that will guide you further down the path:
Reading these next will give you the tools to move from idea to action, so when you’re ready, you’ll already know the best way forward.