Did you know that missed medical appointments cost the U.S. healthcare system over $150 billion every year? If you run in-clinic blood draws, you probably feel that impact daily.
- Patients can’t always get there
- Some live hours away
- Others deal with work, childcare, or unreliable rides
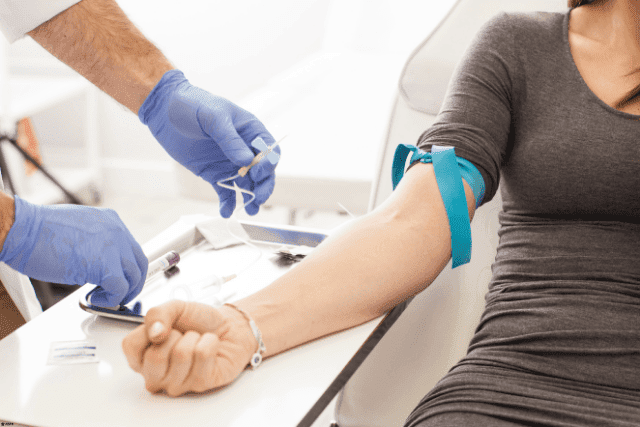
When they don’t show up, your staff loses time, your program loses money, and people miss the care they need. That’s the gap you’re up against. And it raises the big question: Can mobile phlebotomy replace in-clinic blood draws?
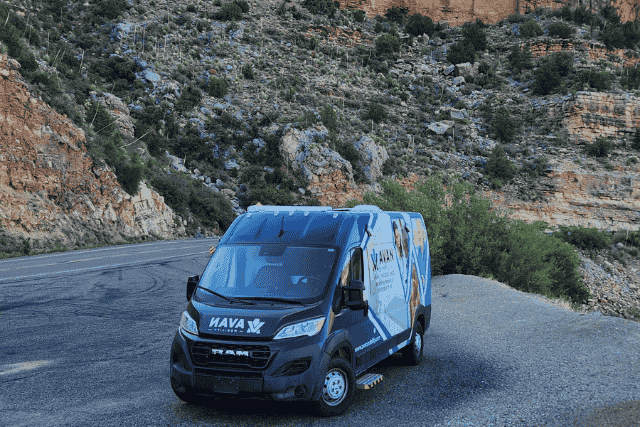
At AVAN Mobility, we’ve spent over 10 years building mobile medical units that help teams like yours close those gaps. We’re trusted by healthcare networks, governments, and non-profits across the U.S. because our vehicles aren’t one-size-fits-all. Each one is built around the real challenges you face.
Our Ford QVM and Stellantis QPro certifications back up our focus on safety and quality. We’ve worked with groups like the Community Clinic of Southwest Missouri and Pacific Clinics to help them bring healthcare into neighborhoods where it’s hardest to reach. And while we’re not the only builder out there, we’ve built our reputation by listening first and designing second.
In this article, you’ll see:
- The problems with in-clinic blood draws
- How mobile phlebotomy services compare
- Key things to know before making a switch
4 problems with in-clinic blood draws

In-clinic blood draws play an important role in healthcare, but they’re often plagued with problems that hold your program back. From missed appointments to patients traveling long distances, the gaps add up. Let’s take a closer look at some of the most common challenges you may be facing.
Problem 1: No-shows drain time, money, and care
If you’ve ever checked the schedule and noticed an empty chair, you know how frustrating no-shows can be. In-clinic blood draws often face this problem. A patient books an appointment, your staff gets everything ready, and then the chair stays empty. It feels like wasted time, but the impact goes far deeper than that.
Every no-show creates a ripple effect:
- Lost staff hours: Phlebotomists and admin staff are left waiting when they could be helping others.
- Wasted resources: Supplies are prepped but not used. That adds unnecessary cost over time.
- Gaps in care: Patients who skip draws don’t get results, which slows down diagnoses and treatments.
Picture a community health program in rural West Virginia. Patients often travel 40 miles or more to reach the clinic. When gas prices spike, some simply can’t afford the trip. The result? Empty appointments, frustrated staff, and patients left waiting longer for the answers they need.
Even large city clinics feel the sting. In places like Chicago, traffic or unreliable public transit can keep people from showing up. When your program depends on keeping a steady flow of patients, every no-show chips away at efficiency, budget, and, most importantly, patient health.
No-shows are inconvenient, drain your resources, stretch your team thin, and leave the people you serve without the care they came for.
Problem 2: Travel barriers can keep patients away
One of the biggest challenges with in-clinic blood draws is that many patients simply can’t get there. The clinic may be hours away for people living in rural or remote areas. Even in cities, the trip can feel overwhelming if someone relies on unreliable transit or struggles with mobility issues. When getting to the chair is harder than the blood draw itself, attendance naturally drops.
Think about what this means for your program:
- Fewer patients served: People who can’t travel stay home.
- Unequal access: Rural communities miss out compared to urban areas.
- Frustrated patients: Long trips for a quick blood draw feel like wasted time.
Take Arizona as an example. Rural counties like Apache and Navajo have vast areas with limited healthcare access. A patient might drive 90 minutes for a five-minute blood draw. If they’re elderly, can’t take time off work, or don’t have reliable transportation, chances are they’ll skip it altogether.
Traffic and parking are major deterrents even in urban centers like Los Angeles. A patient may spend two hours commuting for a ten-minute appointment. That’s not a good use of their time or yours.
Travel barriers leave patients underserved, strain your program’s resources, and create frustration on both sides of the exam chair.
Problem 3: Limited clinic hours create access gaps
In-clinic blood draws often operate on a fixed schedule, typically weekdays from 9 to 5. That works for your staff, but not always for your patients. Many can’t afford to take time off work, find childcare, or arrange transportation during those hours. When your schedule doesn’t match theirs, patients fall through the cracks.
Here’s how limited hours affect your program:
- Missed opportunities: Patients who need draws can’t fit them into their day.
- Delayed results: Care plans stall when patients push tests to “later.”
- Frustrated staff: Cancellations stack up when patients can’t make your timeslot.
Take Houston, for example. Imagine a single parent working two jobs who needs regular bloodwork. They can’t leave during the day without losing wages or risking their job. By the time they’re off work, your clinic is closed. Eventually, they give up on scheduling altogether.
Even in smaller towns, the issue stands out. If your clinic is only open on weekdays, patients may have to choose between healthcare and their paycheck. That’s not a fair choice for anyone.
When your hours don’t line up with the people you serve, access becomes uneven. Patients who can adjust their schedules get care, while everyone else is left behind.
Problem 4: Clinic capacity limits patient flow
Even when patients show up, in-clinic blood draws can run into a different problem: space and staffing. Most clinics can only handle so many people at a time. If too many patients need blood draws on the same day, schedules back up, wait times increase, and your staff ends up stretched thin.
Here’s what happens when capacity becomes a barrier:
- Longer waits: Patients sit for hours, often frustrated before their name is called.
- Burnout risk: Staff feel rushed, stressed, and less able to focus on quality care.
- Lost patients: People may walk out or avoid scheduling in the future.
Think about a busy urban clinic in New York City. Dozens of patients may line up early in the morning, hoping to get bloodwork done before work. By 9:30 a.m., chairs are full, the waiting room is crowded, and staff are already running behind. Patients who can’t wait simply leave, and those who stay may think twice before booking again.
Small-town clinics face the same issue, just on a different scale. With only one or two phlebotomists available, even a small spike in demand can overwhelm the schedule.
When clinic capacity is maxed out, both patients and providers feel the squeeze. It’s a problem that makes scaling your program almost impossible.
How do mobile phlebotomy units compare to in-clinic blood draws?

Mobile phlebotomy units give you another way to serve patients, especially when in-clinic blood draws hit roadblocks. They bring the service to neighborhoods, workplaces, and community centers, meeting people where they are instead of asking them to come to you. Let’s look at how these mobile setups stack up against traditional clinics.
Comparison 1: Mobile phlebotomy reduces no-shows
One of the biggest headaches that we talked about earlier with in-clinic blood draws is no-shows. Patients miss appointments for all kinds of reasons, including transportation, work, or simply forgetting. A mobile phlebotomy unit cuts through that problem by showing up where patients already are. Instead of depending on them to come to you, you meet them halfway.
Here’s how mobile services help:
- Convenient access: Units can park at workplaces, schools, or community centers.
- Fewer barriers: Patients don’t need to juggle travel or long commutes.
- Better attendance: When care is nearby, people are more likely to show up.
Imagine a large employer in Ohio where hundreds of staff need regular bloodwork. When blood draws happen only at the local clinic, no-shows are common because workers can’t leave during their shift. But if your mobile phlebotomy van pulls up outside the workplace, employees can step outside, get their draw, and return to work in minutes. Attendance goes up, results come back faster, and your staff time is used more effectively.
When you’re able to shift the location of “your clinic” to “their neighborhood,” mobile blood draws close the gap left by no-shows. It’s a practical way to save resources, serve more patients, and reduce frustration on both sides of the chair.
Comparison 2: Mobile phlebotomy makes care local
Travel is often the biggest gap between patients and in-clinic blood draws. A mobile phlebotomy unit removes that distance by bringing the service into the community. Instead of forcing patients to plan long drives or juggle complicated bus routes, the unit comes to them on familiar ground.
What this does for your program:
- Cuts down missed care: Patients who couldn’t travel before now have an easy option.
- Levels the playing field: Rural and urban communities get the same access.
- Builds trust: Meeting patients where they live makes your program feel approachable.
Imagine a mobile unit parked outside a public library in rural Georgia. Families already visit the library for community events, so stopping in for a quick blood draw feels natural. There’s no need for time off work, no long road trip, and no stress about finding a ride.
Now, picture the same idea in a big city like Detroit. Instead of battling traffic, patients can walk down the block to a mobile van stationed near a grocery store. What once felt like a major hassle becomes part of an everyday errand.
Mobile blood draws change the equation. Care is no longer “too far away.” It’s right around the corner.
Comparison 3: You can offer mobile phlebotomy services with more flexible hours
Operating on a 9-5 schedule can make it tough for people to get to a fixed clinic. A mobile phlebotomy unit adds flexibility by going where and when people need it.
Here’s what flexible service looks like:
- Evening availability: Vans can operate after regular work hours.
- Weekend coverage: Community events and Saturday visits bring in more patients.
- Custom scheduling: Programs can target workplaces, schools, or senior centers at times that fit best.
Think about a manufacturing plant in Indiana where most employees work 12-hour shifts. Traditional clinic hours never align with their availability. When a mobile phlebotomy van shows up outside the plant at 6 a.m. before a shift, employees can get bloodwork done without missing work. Attendance spikes, care stays on track, and your program keeps running smoothly.
In suburban communities, weekend events offer the same advantage. A mobile unit parked at a Saturday farmers market in North Carolina can serve dozens of patients who would otherwise push off bloodwork until “later.”
When you expand care beyond clinic hours, patients stop feeling boxed in by schedules. Flexible mobile phlebotomy services make blood draws fit into daily life instead of forcing life to fit the clinic.
Comparison 4: Mobile phlebotomy can expand patient capacity
Mobile phlebotomy units expand your reach by creating extra capacity outside of your building. Instead of being stuck with the four walls of a clinic, you can bring care to more places at once.
Here’s how added capacity plays out:
- Shorter waits: Patients don’t crowd into the same location.
- Scalable programs: Multiple units can serve different sites on the same day.
- Efficient flow: Staff manage a steady pace instead of overwhelming rushes.
Picture a health network in Texas managing both rural and suburban clinics. Their central lab gets swamped every Monday morning, with long lines and frustrated patients. When they started deploying two mobile blood draw vans to nearby towns, they cut the load in half. The clinic runs smoothly, patients spend less time waiting, and staff feel less overwhelmed.
Even small organizations can benefit. A community health program in Maine might add a mobile unit to cover local senior centers. Instead of everyone arriving at the same clinic on one day, patients are spread across several easy-access sites.
Mobile phlebotomy services break through the capacity ceiling, giving you more ways to serve more people without overloading your clinic.
Other benefits of mobile phlebotomy compared to in-clinic blood draws

While mobile phlebotomy units solve big issues like no-shows, travel, and scheduling, there are other benefits worth noting. Here’s a quick side-by-side look at some advantages that often get overlooked:
| Benefit | How it helps |
| Community visibility | Units parked in public spaces raise awareness and normalize preventive care. |
| Patient comfort | People feel less anxious stepping into a smaller, private van versus a crowded clinic. |
| Outreach opportunities | Mobile units can double as educational hubs for wellness checks and health info. |
| Brand trust | Programs seen actively showing up in neighborhoods often gain stronger community support. |
| Faster program growth | Adding a mobile unit can expand reach without the long delays of building new facilities. |
| Data collection | On-site registration helps gather valuable insights about underserved areas. |
| Emergency response | Units can pivot quickly to serve communities hit by disasters or sudden health crises. |
| Reduced patient costs | Patients save money on gas, parking, and childcare by accessing care closer to home. |
Mobile phlebotomy opens up new ways to connect with people, strengthen your program, and grow trust in the communities you serve.
Considerations to determine if mobile phlebotomy is the right fit
A mobile phlebotomy unit sounds promising, but it’s not the right solution for every program. Before making the switch, here are some wise questions to ask yourself:
- Patient population: Do most of your patients live far from your clinic or struggle with reliable transportation? If so, mobile phlebotomy services may close that gap. If your patients are mostly nearby with easy access, in-clinic blood draws may still work well.
- Volume of need: Are missed appointments or long wait times cutting into your efficiency? Mobile blood draws can add capacity and reduce no-shows, but if your appointment books aren’t full, you may not need the investment.
- Private setting: Would your patients feel more comfortable seeing care offered in a private mobile clinic instead of a busy doctor’s office or hospital? If yes, a mobile option could build trust and visibility.
- Budget and resources: Do you have the staff, funding, and logistics to operate outside the clinic? Mobile units require planning for routes, staffing, and supplies.
- Long-term goals: Is your mission to grow reach, reduce barriers, and expand access into underserved areas? If that’s part of your strategy, mobile phlebotomy could be a strong fit.
Thinking through these factors helps determine whether a mobile unit should replace or simply complement your in-clinic blood draws.
Ready to start your mobile phlebotomy journey?

You came to this article because you might be dealing with challenges like no-shows, travel barriers, rigid clinic hours, and limited capacity. These problems create real strain on your staff, your budget, and the patients who depend on you.
Here’s what you’ve learned today:
- The biggest problems tied to in-clinic blood draws
- How mobile phlebotomy services compare and help fill those gaps
- Additional benefits and smart considerations before making the switch
At AVAN Mobility, we design vehicles with one goal in mind: Helping healthcare teams like yours remove barriers to care. For more than a decade, we’ve worked on building units that don’t just look good on paper; they make a real difference in people’s lives. Each mobile medical van we build is shaped by listening first and tailoring second.
That’s why so many of our partners stay with us long after their first unit hits the road. We know the stakes are high, and we’re proud to stand alongside you as you bring healthcare closer to the people who need it most. If you’re ready to take the next step, click below to talk with a mobility expert today.
If you’re not ready to talk just yet, here are a few articles that will guide you further:
1. How much does a mobile medical unit cost in the U.S.? Understand the financial side of going mobile.
2. Buying a mobile medical van: Learn what the journey looks like from idea to delivery.
3. How to apply for mobile health grants: Discover practical ways organizations fund these projects.
Reading these next will give you a clearer picture of costs, processes, and funding assistance so you can move from exploring mobile phlebotomy to actually making it part of your program.