Ever wonder how IHS facilities in Arizona and across the U.S. keep up with rising healthcare needs when their clinics are hours apart and staff are stretched thin? It’s a tough spot. According to the IHS, Native communities face higher rates of diabetes, heart disease, and more. Add long distances, limited transportation, and overworked staff, and it’s no surprise people sometimes skip care.
That gap is serious.
It often means:
- Delayed diagnoses
- Worsening health
- In some cases, lives are cut short
The better way? Bring care right to these communities with mobile medical units so they stay healthier and longer.
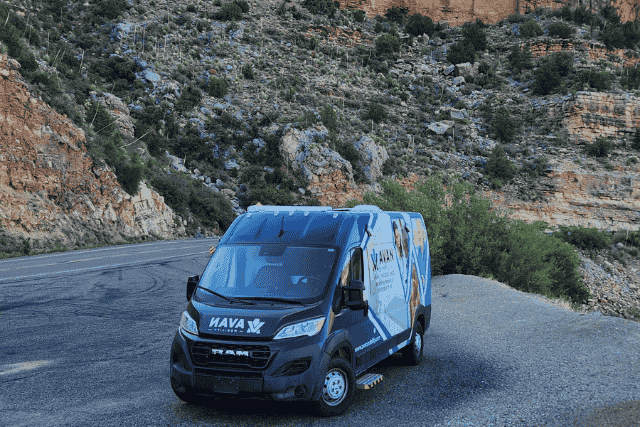
I’m Simon Jones. I’ve been with AVAN Mobility for almost 15 years, starting as a technician. I eventually moved into customer service and found my passion for helping people. Now, I work alongside tribes and healthcare teams to figure out what mobile units fit best. We’ve done this for over a decade, building vans that break barriers and save lives.
In this article, I’ll explain how IHS facilities use mobile medical units so you can better determine whether they’re the right fit for your community.
How do IHS facilities in Arizona use mobile medical units to close healthcare gaps?
Let’s be real. IHS facilities across Arizona, and honestly, the whole country, are stretched. You’ve got federal IHS facilities trying to serve huge areas with small teams. Many brick-and-mortar clinics sit hours apart. Patients who don’t have a ride or can’t take time off work end up skipping care. That gap hits hard. It can turn a simple wound into an infection or mild diabetes into a life-changing problem.
I’ve seen it firsthand. When I work with IHS facilities in Arizona, it’s clear these teams care deeply; they just need more tools. That’s why so many are adding mobile medical units to their lineups. They can roll into a village, park at a school, or set up at a local event. Suddenly, people who felt forgotten have a nurse or doctor right there.
Here’s how these units often help:
- Chronic disease care: Manage diabetes, hypertension, and asthma without long drives.
- Screenings: Catch cancers or heart risks early so they don’t turn into bigger nightmares.
- Dental services: Keep infections and tooth loss at bay because we all know dental pain is brutal.
- Behavioral health: Offer counseling or group sessions in a private, familiar space.
- Diabetes support: Help folks stay on top of blood sugar checks, foot care, and medication tweaks so complications don’t sneak up.
- Rehabilitation: Bring therapy closer to home, from post-op recovery to stroke rehab, so patients don’t miss crucial appointments.
- Health education: Host workshops on nutrition, managing chronic conditions, or even parenting tips right in the community, which makes learning much easier.
Next, I’ll show you why even federal IHS facilities that already have fixed clinics see mobile medical units as game changers.
Why do federal IHS facilities still see the need to invest in mobile medical units?

You might wonder, if federal IHS facilities already have brick-and-mortar clinics, why bother with mobile medical units? Fair question. Truth is, even staffed clinics can’t always keep up. Many sites in Arizona and other parts of the country are booked solid. It’s tough enough to snag an appointment for a routine check, let alone squeeze in urgent care when something flares up.
I hear it all the time when talking with program directors. They’ll say, “Simon, our clinic’s full, and we’re miles from the next nearest facility. We can’t just tell people to wait three weeks.” That’s exactly where mobile units come in. They help IHS facilities handle overflow and reach patients who might otherwise slip through the cracks.
A few smart ways I’ve seen federal IHS facilities use mobile medical units include:
- Seasonal deployments: During flu season or vaccination drives, a mobile unit can park closer to where families live, saving them hours of travel.
- Event-based care: At powwows or tribal fairs, these units can quietly do screenings and blood pressure checks while folks are already gathered.
- Specialty days: Some bring in specialists a few days a month, setting up cardiology or women’s health clinics right on wheels.
That flexibility is gold. It means more people get seen faster, which prevents small issues from blowing up into serious hospital visits. It also shows community members that IHS facilities in Arizona and beyond are willing to meet them halfway, which goes a long way in building trust.
Up next, let’s take a look at that number of IHS facilities again and why that number proves mobile medical care is a smart move.
How many IHS facilities are there?
So, how many IHS facilities are there? Across the U.S., about 600 IHS and tribally operated facilities. That might sound like a solid number at first. But then you realize they’re spread out over 574 federally recognized tribes and some of the most wide-open spaces you’ll find anywhere.
It’s no surprise IHS facilities in AZ lean on mobile medical units. They keep folks healthier, cut ER visits, and give communities a sense that someone cares enough to come to them.
Suddenly, that number feels a lot smaller.
Take Arizona, for example. There are dozens of IHS facilities in Arizona, but they’ve got to cover communities scattered over hundreds of miles. A clinic might serve multiple reservations. That means patients sometimes drive hours for routine care. For folks juggling jobs, kids, and unreliable cars, that can lead to putting off visits until things get worse.
Here’s why that matters:
- Long gaps: With so few sites, many families simply don’t go, which can let chronic problems spiral.
- No quick fixes: Adding permanent clinics takes years and big budgets.
- Mobile is fast: A mobile unit can start seeing patients within months, right where they live.
When I work with federal IHS facilities, we often talk about this exact numbers game. They’ll say something along the lines of, “Simon, we’re doing our best, but we’re spread thin.” That’s where mobile medical units shine. They don’t replace clinics. They stretch their reach so more people get help before it’s an emergency.
Next, let’s look at some of the clever ways IHS facilities in AZ are actually putting these mobile units to work so you can see what’s possible.
How IHS facilities in AZ, like Chinle, use mobile units to reach more people

Alright, so let’s put all this talk into something real. One of the IHS facilities in Arizona we’ve worked with is Chinle Health Care Facility. They serve a huge part of the Navajo Nation, which, if you’ve ever driven through, you know, isn’t exactly around the corner. We’re talking about long stretches of desert and canyon country that are stunning but tough if you’re trying to get to a clinic.
When Chinle added a mobile medical unit, it wasn’t just a fancy new toy. It was a lifeline. They can now roll out to more remote chapters, cutting the need for families to drive hours for a simple checkup. That means fewer missed appointments, fewer small problems turning into big emergencies, and more people catching chronic issues early.
Here’s what this looks like on the ground:
- Community screenings: Set up at chapter houses so folks can get their blood sugar and blood pressure checked close to home.
- Follow-up care: Patients who had to wait weeks for the clinic can hop into the van that visits their area twice a month.
- Health fairs: During big gatherings, their mobile team does quick consults and hands out health info on the spot.

When I talk to organizations like Chinle, it’s clear these mobile clinics are more than steel and wheels. They’re trust builders. They show people that IHS facilities in AZ care enough to come to them, no matter how far out they live.
Next, I’ll wrap this up by talking about how mobile units strengthen relationships, which is sometimes the biggest win of all.
How do mobile medical units help IHS facilities build trust and strengthen communities?
At the end of the day, most people don’t think about IHS facilities in terms of how many there are or which are federal. They think about who shows up when they’re worried about a lump, struggling to breathe, or scared for their kids. That’s where mobile medical units pull more weight than you’d expect.
I’ve seen it over and over, especially with IHS facilities in Arizona. When a big clinic feels intimidating, a van parked right in someone’s neighborhood comes off way more approachable. Folks who might skip out on care walk up just to see what’s happening. Before you know it, they’re chatting with a nurse, getting their vitals checked, or scheduling a follow-up.
Why does this matter?
- Trust grows: People see healthcare workers right there in their community, which makes them more likely to come back.
- Small steps turn big: Someone might start with a blood pressure check, then open up about other health concerns they’d been ignoring.
- Relationships build: The more these vans roll through, the more families view the staff as neighbors, not strangers.
When I talk with directors at federal IHS facilities, they’ll often tell me the real win isn’t just more appointments. It’s the stories of a grandmother who finally manages her diabetes or a teenager who gets counseling before depression spirals. That’s the power of showing up consistently.
I sometimes like to think of mobile medical units as bridges. They connect communities to care, one stop at a time.
What’s next?
You probably came here because, like so many leaders at IHS facilities, you’re worried about long drives, missed appointments, and patients slipping through the cracks. That initial challenge is heavy, and nobody wants to see chronic diseases worsen just because care is out of reach.
Here’s what you picked up from this article:
- How IHS facilities in Arizona and all over use mobile medical units to bridge long distances
- The smart ways federal IHS facilities make mobile care stretch limited budgets
- Stories that prove these vans don’t just deliver care, they build trust and relationships
At AVAN Mobility, we’ve helped organizations from tiny tribal clinics to major health networks figure out what kind of mobile unit truly serves their people best. We’ve fine-tuned hundreds of vans over the years to handle dusty roads, tight village layouts, and specialized care setups.
Seeing a mobile clinic drive up and patients breathe easier is why I keep doing this. It’s also why we’re trusted leaders in the industry. If you’re curious or just want to bounce ideas around, click the button below, and let’s chat.
If you’re not ready to talk yet, here are some other helpful articles to keep exploring:
- Top 10 tips on fundraising for a Mobile Clinic Van: Perfect if you’re starting to think, “How would we even pay for this?”
- Buying a mobile medical van: Your process with AVAN Mobility: This one shows what you can expect, so nothing feels overwhelming.
- Top 7 ways to apply for mobile health grants: Great if you’re looking for grant money to help get your mobile clinic rolling.